SK-HEP-1 Cell Line Derived Xenograft
SK-Hep-1 is a human hepatocellular carcinoma (HCC) cell line commonly used in research to study liver cancer, particularly hepatocellular carcinoma. The SK-Hep-1 cell line was originally derived from a patient with liver cancer. Subcutaneous xenografts are the most widely used preclinical models for cancer therapeutics. The SK-HEP-1 cell line derived xenograft (CDX), with mutations in BRAF and CDKN2A, rapidly forms subcutaneous tumors that can easily be measured by calipers to determine therapeutic efficacy. Along with its use in monotherapy or combination therapy approaches, the SK-HEP-1 CDX model is utilized in studies addressing the mechanism of action or reduction of tumor growth (e.g. ABT-869 or rapamycin).
| SK-HEP-1 Mutations | BRAF(mut), CDKN2A(mut) |
| Origin | Liver |
| Disease | Adenocarcinoma |
| Metastatic Models (Liver) | SK-HEP-1 |
| Non-Metastatic Models (Liver) | H22, Hepa1-6, Hep3B, HepG2, Huh7, SMMC-7721 |
Metastatic Model
Proliferating tumor cells invade local tissue, travel through the circulatory system and implant in a foreign tissue. Metastasis leads to high death rates in cancer patients. Cell line derived xenograft (CDX) mouse models are highly utilized in preclinical assessment of novel cancer therapeutics and are a crucial link between initial high-throughput in vitro screening data and anti-tumor efficacy. Metastatic mouse models are utilized to understand the interactions of the anti-metastatic therapeutic and tumor in regards to all organs, bioavailability (e.g. half-life), clearance, immune response and tumor efficacy. Due to the inability to palpate metastatic tumors, the insertion of a luciferase (bioluminescence) or GFP (fluorescence) gene into the genome of the cell line of interest enables the researcher to visually track and quantitate internal tumor progression throughout the in-life portion of the animal study.
U87-Luc MG Xenograft Model (case study)
U-87 MG cells expressing luciferase were implanted and the tumors were allowed to grow. Using a Night Owl (Berthold Technologies), tumor growth was monitored throughout the study after an intraperitoneal (IP) injection of luciferin. An image of tumor location and the ability to capture a quantifiable value for orthotopic or metastatic tumor progression is the main strength of the luciferase expression (emitted photons) in the U87 MG-Luc model.
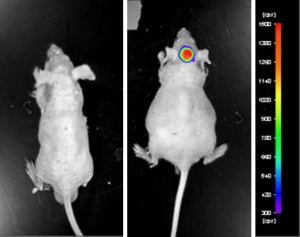
Figure: Expression of luciferase in U87-Luc MG orthotopic model. Control (left) and implanted glioma mouse model fluorescence (right) was captured after intraperitoneal luciferin injection (10 min incubation).
View details of the case study here.
Get Instant Quote for
SK-HEP1 Xenograft Model
What is a Xenograft?
Development of an anti-cancer therapeutic requires intense, well planned studies that follow a streamlined path for success. Primary studies are performed in an in vitro setting that allows for high throughput screening and analysis of multiple compounds of interest. This method enables a focused compound screening approach of multiple cell lines within a specific cancer type, or a divergent approach across a broad range of cancer types. Ultimately, in vitro screening results need to be confirmed in an animal model due to in vitro inadequacies of cells cultured on plastic, as this method is far removed from the microenvironment of a tumor.
As the logical next step in therapeutic development is the administration of the test compound in a living animal, a cell line derived xenograft model (CDX) is created by inoculating human cancer cell lines in test animals. The injected cell lines grow into established tumors, thus, permitting efficacy studies of the test compounds. An alternative to CDX models is the patient derived tumor xenograft (PDX) which consists of implanting human tumor fragments directly in a mouse model. The PDX model avoids concerns with the CDX model since the tumor is never grown on plastic and there is no selection for single cell populations. In contrary to CDX models, the ideology of PDX models is to maintain the cell population, structure and stroma of the initial tumor.
Why use Xenograft Models?
Cell line derived xenograft (CDX) models or patient derived tumor xenograft (PDX) models enable a larger realm of parameters to be studied not capable with in vitro studies. The complete animal system model expands the scope of studies available to include the effect of test compounds on pharmacokinetics (PK), pharmacodynamics (PD), alternate routes of delivery, inhibition of metastasis, CBCs, dosing regimens, dose levels, etc. However, one of the major drawbacks of CDX and PDX models is that the human cancer cell lines or human patient derived tumors must be implanted in immunocompromised mice in order to bypass the graft versus host rejection by the animal. With the increasing focus of the immune systems role in the recognition and elimination of tumor cells (i.e. immunotherapy), major consideration must be taken into account during experimental concept design of the limitation of checkpoint inhibitors or desired immune response involvement in tumor efficacy. Similarly, any tumor regression after treatment with a test compound in these models will not exhibit the potential complement cascade or innate immune response of the injected therapeutic in humans.
What we offer?
Our in vivo xenograft service department evaluates the efficacy of preclinical and clinical cancer therapeutics utilizing more than 50 validated immunocompromised xenograft mouse models. The value of utilizing our xenograft service department is highlighted by the ability to completely characterize the efficacy, dose regimen, dose levels and optimal combination ratios of lead compounds for cancer, obesity, diabetes, infections and immunology research.
During the design and execution of the xenograft study, our scientists will communicate with and assist the client’s decisions regarding these details:
- Study Group Formation: classification of mice by body weight, tumor size or other parameters
- Cancer Cell Line: use of in-house cell lines or utilization of customer-provided cell lines
- Tumor Implantation: intraperitoneal, subcutaneous, submuscular or intravenous
- Test Compound Administration: intraperitoneal, intravenous, tail vein, subcutaneous, topical, oral gavage, osmotic pumps or subcutaneous drug pellets
- Sample Collection: Tumors/tissues can be fixed in 10% NBF, frozen in liquid N2 or stabilized in RNAlater; blood chemistry analysis can be performed throughout the in-life portion of study
Vivarium
Our vivarium is designed such that it enables cost-effective and first-rate preclinical effectiveness testing services. All animal handling and maintenance is regulated following IACUC guidelines. Our facility consists of the following:
- IACUC-regulated and GLP-compliant
- Controlled, limited access lab areas
- Disposable cages
- Sterile food and water
- SPF (specific pathogen-free) animals to guarantee pathogens do not interfere with the experiment
- Established animal handling and micro-injection equipment systems, including an animal health observation program
- All studies follow pre-approved SOPs
Our staff understands that each proposed study design is unique and customized to the client’s needs. We also recognize the importance of the delivered results as being confidential, highly reproducible and that 100% of the intellectual property (IP) is owned by the client.
In order to receive a quote for your xenograft study, email us the specific details listed below in order to efficiently begin the study quote process:
- Cancer cell line(s) used in the study
- Number (n=) of animals in each study group
- Number of study groups and control groups
- Tumor implantation route
- Administration route of test compound
- Species of immunocompromised mouse (e.g. NOD/SCID, athymic Nude)
- Treatment and dose schedule
- Study endpoint and analysis (e.g. tumor growth delay, PK/PD, survival, toxicity, drug combinations)
- Samples collected: tumor and tissues to be collected, including storage condition (e.g. snap frozen, RNA-later, 10% NBF, nucleic acid isolation)